This post was contributed by Dr. Mario Elia. The original entry can be found on his blog at https://drmarioelia.wordpress.com
Back in December 2016, I was doing some work around proton pump inhibitor (PPI) costs in Ontario and did some digging into my EMR data to see what savings could be found.
Here was my Twitter thread about the topic.
In short, I identified 414 of my patients on a PPI, 314 (76%) of which were on rabeprazole or pantoprazole, the two cheapest options. I calculated the potential monetary savings by switching every patient in my practice who is on a more expensive PPI (esomeprazole, lansoprazole, omeprazole, dexlansoprazole) to generic rabeprazole; projected tally would be $22,340 over the course of a year. Not an insignificant sum.
It’s one thing to project a cost savings. But would it actually work?
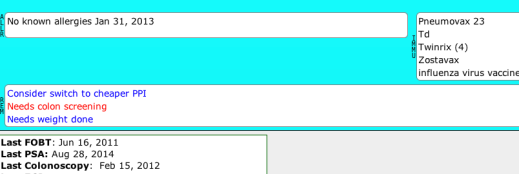
I embarked on a very simple intervention in January 2017. Using my EMR (Telus PS Suite), I created a reminder that would place the note “Consider switch to cheaper PPI” on the chart of every patient on esomeprazole, lansoprazole, omeprazole, dexlansoprazole, or pantoprazole.

That reminder would appear on their chart, and would prompt a discussion at their next appointment about a potential trial of rabeprazole.
(I am intentionally omitting the issue of de-prescribing from this analysis, as de-pescribing PPIs has been another important undertaking in my practice, yet this analysis was strictly looking at looking at cost-saving from cheaper PPIs. The above reminder did prompt many instances of de-prescribing, but these were not as easily quantifiable retrospectively. In addition, I bristle at the idea of openly quantifying and applauding the cost savings from de-prescribing, as it would rightfully raise the question in patients’ eyes whether we are de-prescribing out of concern for their health, or simply to save money. This analysis looks at cost-savings from switching from one PPI to another, the goal of which is to produce no clinical negative change).
Of the patients who were engaged in a discussion, many were found not to be appropriate for a rabeprazole trial, either because of intolerance or lack of efficacy from previous trials of rabeprazole. Other patients were not open to a trial because of lack of interest in “rocking the boat” or because of an upcoming trip and concern about impacting travel insurance.

28 patients (some private pay, some publicly-funded) who required ongoing PPI therapy (due to ongoing indication or due to previous failure with PPI wean) agreed to a rotation to rabeprazole as a trial. 7 patients described a clinical worsening of symptoms (most within the first two weeks), and requested to be put back onto their initial PPI (5 patients on lansoprazole, 1 on pantoprazole, and 1 on omeprazole). 21 patients saw no clinical change, and those 21 have been found to be stable at the 3-month mark post-rotation (11 on lansoprazole, 4 on omeprazole, 4 on esomeprazole, and 2 on pantoprazole).
The cost savings were as follows (using rabeprazole 20mg tablet, $0.24/pill):
- Esomeprazole – $1.86 per pill ($1.62 savings/d, $591.30/yr per patient)
- Omeprazole – $0.41 per pill ($0.14 savings/d, $51.10/yr per patient)
- Lansoprazole – $0.50 per pill ($0.26 savings/d, $94.90/yr per patient)
- Pantoprazole – $0.30 per pill ($0.06 savings/d, $21.90/yr per patient)
Total yearly savings from these 21 patients now stable on rabeprazole: $3657.30
A few things to take away from this:
- This was a ridiculously simple intervention, and took me virtually no time to create the reminder or to have those discussions with patients.
- This should be a wake-up call to the Ministry of Health on the importance of working with physicians on finding efficiencies in our system. Physicians know where these efficiencies are, so allow innovation and creativity, reward it appropriately, and we’ll find the money.
- It is critical that the first script for the rabeprazole be of short duration (I prescribed two weeks), otherwise 3 months of wasted pills for the 25% failure rate would have erased some of the cost savings.
- Most practices will likely see greater savings than I achieved in my practice, as I have been consciously working to prescribe exclusively rabeprazole for some time now. Even if you assume my prescribing rate to be on par with the Ontario average (2200 patients), extrapolating this out to Ontario’s population of 13.6 million, this simple intervention would amount to a provincial total of $22.6 million.
- Note that most of the savings were found in switching patients from esomeprazole. Please don’t use it unless you are absolutely handcuffed. It is insanely expensive compared to others in the class.
All of us have these opportunities in our practices for small interventions that we may actually find some element of satisfaction in evaluating, especially with the power of a well-functioning EMR behind us.

